Lisa Qiu1, Irene Young1, Christopher Hernandez1, Christina Kim1, Robyn Dreibelbis DO1
PNWMSRJ. Published online Sept 6th, 2020.Abstract
Chronic diseases are estimated to cost the United States nearly 84% of its health care sector spending. The Complete Health Improvement Program was founded in 1988 in an effort to decrease the prevalence of chronic diseases, and consequently lower the cost of health care. The Complete Health Improvement Program was implemented at Samaritan Lebanon Community Hospital in Lebanon, Oregon, from January 2016 to December 2018, resulting in six courses and totaling 104 participants. Out of 104 participants, 81 participants obtained pre-course and post-course vital signs or laboratory blood work. Using the pre-course and post-course values, this study aims to analyze the short-term effectiveness of the Complete Health Improvement Program at Samaritan Lebanon Community Hospital. Results showed significant decreases in cholesterol (p-value <0.001), high-density lipoprotein (p-value <0.001), low-density lipoprotein (p-value <0.001), systolic blood pressure (p-value <0.001), diastolic blood pressure (p-value <0.001), weight (p-value <0.001), and fasting glucose (p-value <0.004). Additionally, non-significant decreases in triglycerides (p-value <0.3) and very-low-density lipoprotein (p-value <0.4) were observed. Overall, the Complete Health Improvement Program, which revolves around a plant-based diet along with an emphasis and education on personal lifestyle choices to overall health, shows a positive short-term reduction in risk factors that contribute to chronic diseases within the Samaritan Health Services and the population it serves.
Introduction
Towards the end of the 20th century, the focus of healthcare shifted from acute treatments and infectious diseases to chronic diseases such as hypertension, diabetes, and cardiovascular disease. These chronic conditions became more prevalent, while many acute illnesses became curable with advancements in medical research. In 2009, it was estimated that 145 million people lived with at least one chronic condition, and spending associated with managing those conditions accounted for 84% of health care spending.1 With the rising cost of health care and the overwhelming financial burden that chronic diseases have on the national budget, it is crucial to implement programs to lower its prevalence.
The Complete Health Improvement Program (CHIP) was founded by Dr. Hans Diehl in 1988 to combat the rising prevalence of chronic diseases, many of which contain underlying components that are related to lifestyle choices, such as diet and exercise. It has been shown that numerous chronic diseases are responsive to lifestyle modifications.2 The CHIP aims to implement those changes with emphasis on a plant-based diet, nutritional education, and importance of personal lifestyle choices.
The CHIP at the Samaritan Lebanon Community Hospital (SLCH) in Linn County of Oregon started in January 2016. One full CHIP course consists of 18 bi-weekly classes over a span of nine-weeks. Each class focuses on different components of plant-based diets and other lifestyle determinants of health like exercise, stress reduction, sleep, relationships, etc., that can be incorporated into patients’ lives.
Six CHIP courses have been started at SLCH where 104 participants enrolled with the most recent class ending in December 2018. Every community has unique needs and resources, making it necessary to personalize certain aspects of the generalized CHIP curriculum. This study attempts to understand whether the participation and completion of the CHIP course benefitted the community through a thorough analysis of laboratory values and vital sign measurements.
To evaluate the short-term effectiveness of the CHIP curriculum for Linn County, an analysis of the participants’ lipid panel, fasting glucose, and vital signs was performed with the following question in mind – ‘Does completion of the CHIP course lead to improvement in the laboratory values and vital signs?’
Given the structure of this course, and the results of previous research on CHIP, it is expected that all values would show positive short-term health benefit of the program upon completion of the CHIP.3,4,5,6
Methods:
All participants were asked to make a laboratory appointment within the week prior to the start of the course up until the second class. Once individuals were able to attend 12 or more of the 18 classes, participants were categorized as “completed” for the CHIP course and asked to schedule a post-course laboratory appointment. The post-course values were taken anytime during the last week of classes until three days after the last class. The flexibility of these timeframes was made to accommodate participants’ schedules. Vital signs collected include systolic and diastolic blood pressures and weight. Laboratory work included triglycerides (TG), total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and very-low-density lipoprotein (VLDL), and fasting glucose.
All subjects met the following inclusion criteria: (1) enrolled and attended at least 12 of 18 classes of the CHIP course at SLCH between January 2016 to December 2018; (2) obtained a pre-course and post-course set of vital signs or a pre-course and post-course set of laboratory blood work, or both. Subjects were excluded from the study based on the following exclusion criteria: (1) enrolled but did not complete the CHIP course; (2) failed to obtain a pre-course and post-course set of vital signs and a pre-course and post-course set of laboratory bloodwork. Of the participants included in the study, participants were excluded from specific categories of analysis due to the following: (1) non-fasting or ambiguous fasting status made them ineligible for TG and fasting glucose calculations; (2) non-numerical laboratory or vital sign values; (3) missing a pre-course or post-course value. Twenty-three participants were excluded in certain categories. Table 1 presents those categories and the explanation for their exclusion.
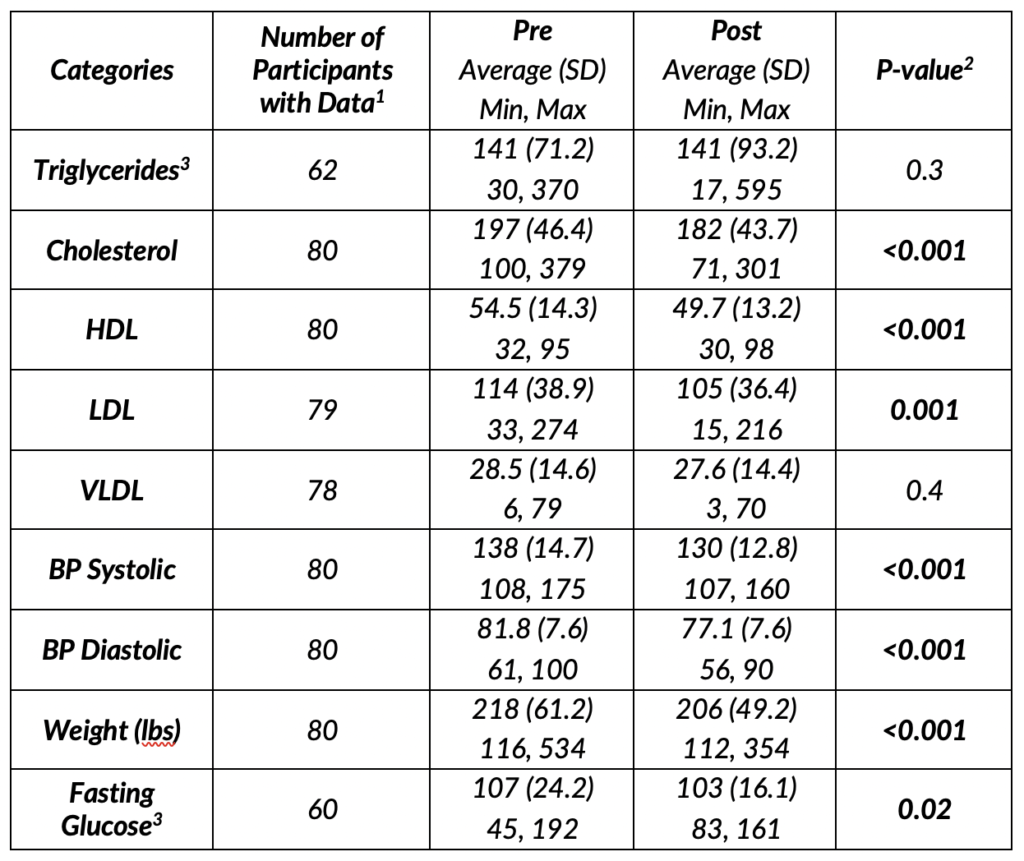
Table 1. Explanations of special circumstance of exclusion for certain categories for Participants 1 through 23.
A retrospective chart review was performed on participants based on the inclusion and exclusion criteria. Of the 104 participants enrolled, 86 completed the CHIP course and 81 were included in this dataset for analysis. Blood pressure, weight, fasting glucose, and lipid panel data were compared from before to after the CHIP course using paired t-tests for normally distributed variables, and Wilcoxon signed-rank tests for non-normally distributed variables. Participants who were missing pre or post data for a given variable were excluded from that analysis. All analyses were performed in R version 3.6.1.
Results:
Based on the data of pre-course and post-course measurements of participants enrolled in the CHIP at SLCH, there were statistically significant reductions in TG, cholesterol, HDL, LDL, BP systolic, BP Diastolic, and weight. There was also a reduction of average cholesterol values from 197 to 182 (p-value <0.001), average HDL values from 54.5 to 49.7 (p-value <0.001), average LDL values from 114 to 105 (p-value 0.001), average BP systolic values from 138 to 130 (p-value <0.001), average BP diastolic values from 81.8 to 77.1 (p-value <0.001), and average weight from 218lbs to 206lbs (p-value <0.001).
There were statistically non-significant reductions in TG, VLDL, and fasting glucose. TG was noted from 141 to 141 (p-value 0.3), VLDL from 28.5 to 27.6 (p-value 0.4), and fasting glucose from 107 to 103 (p-value 0.02).
A detailed table of the average pre-course values, average post-course values, participant number, and p-values can be seen in Table 2.
Discussion:
Overall, each category showed a decrease in average value at the end of the CHIP compared to average values at the start of the course. Two of those categories, TG and VLDL, had a non-significant decrease over the nine-week period. The overall decrease in lipid panel categories, blood pressure, and weight, show support for the positive effects of short-term effectiveness in improving one’s health with the implementation of a plant-based diet.
Interestingly, the dataset shows a decrease in HDL stores in the 80 participants in this study after the CHIP course. HDL has long been associated as “good cholesterol” due to its ability to carry cholesterol from the periphery of the body back to the liver.
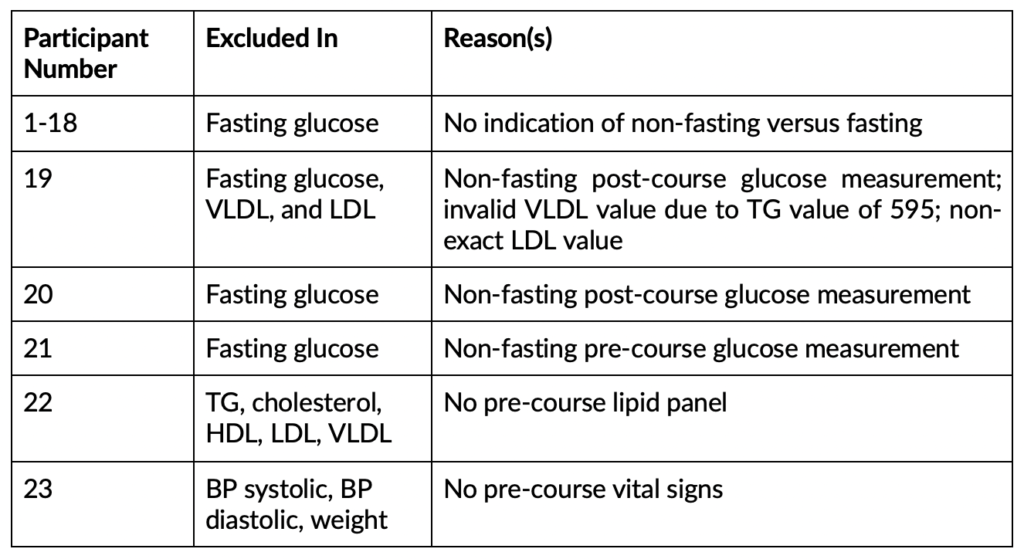
Table 2. Statistical analysis results for each category with the number of participants, pre-course average value, post-course average value, and p-value.
2P-values for cholesterol, LDL, BP Systolic, and BP Diastolic were from paired t-test with equal variance, p-values for TG, HDL, VLDL, weight, and fasting glucose were from Wilcoxon signed rank tests due to a non-normal distribution.
3Participants who were not clearly designated as “fasting” for their glucose measure were excluded.
Levels of HDL has been reported to have an inverse relationship with the incidence of coronary heart disease (CHD). Notably, while low HDL is not a cause for CHD, it has been identified as an independent predictor of risk for CHD.7,8 The results of this study indicate significant short-term reduction in HDL stores in participants, which may raise concerns for potential secondary risk in developing CHD. However, studies that report low HDL being an independent predictor of CHD have also tied low HDL to unhealthy lifestyles in individuals with high TG, cholesterol, LDL, VLDL, and other comorbidities that contribute greatly to poor cardiovascular function.9 To complicate matters, a cohort study of 3590 men and women from the Framingham Heart Study showed cardiovascular disease (CVD) risk associated with low HDL, but more so in individuals accompanied by LDL >= 100mg/dL and/or TG >= 100mg/dL. The study further found that low HDL in isolation is a considerably less predictive of CVD risk when there is high TG, high LDL, or both.10 Hence, it is difficult to interpret the findings of low-HDL levels in individuals without looking broader at their overall lipid panel, which in this study shows significant reduction in categories that are often more greatly associated with cardiovascular compromise.
Notably, the significant decreases in cholesterol, LDL, VLDL, BP systolic, BP diastolic, weight, and fasting glucose after completion of the CHIP is indicative of better overall health of the participants within nine weeks. A complicating factor in this analysis resides in the differences in the timeline of the recording of the individuals’ vital signs and laboratory work. The flexibility of timeframes could have potentially generated a maximum of a 10-day difference between the earliest participant and the latest participant. When evaluating the short-term effectiveness of the CHIP, a 10-day difference may have a significant effect in the outcomes of their laboratory and vital sign values.
Overall, some of the biggest limitations in this study remains to be the bias of the sample population and sample size. While the sample size is adequate (n = 81), there was a portion of participants that were not accounted for in the fasting glucose and TG calculations due to aforementioned circumstances, which lessens the power of those categories. Individuals were often encouraged by their primary care providers to join the course due to their pre-existing health diagnoses. In addition, individuals who enrolled may be actively attempting to change their lifestyles and be more motivated than the average individual. Individual motivation continues to factor into other aspects of this study, such as those who were willing to come back to get their labs drawn and vital signs taken and those who did not complete the course were not accounted for.
In this study, participants in the course was limited to individuals with financial stability. The cost of the program is $650 where only current Samaritan Choice and Intercommunity Health Network insurance plans will cover the CHIP course. Individuals who were able to afford the program may have been more motivated than the average person to change their lifestyles.
One of the most challenging components in evaluating the effectiveness of the CHIP course is accounting for the degree of changes that individuals make in their diet and lifestyle using the education they received during the course. One individual may start a plant-based diet immediately after the first class compared to another individual starting midway through the course. Other participants may slowly incorporate more plant-based meals into their diet and variations of participant diets are infinite. It is not a requirement for participants of the program to be on a strict plant-based diet throughout the nine-weeks with routine exercise scheduled. As a result, there is a possibility that some individuals never changed their diet or changed it to incorporate more unhealthy habits. However, the portion of individuals that made negative changes in their lifestyle is likely in the minority, due to the aforementioned discussion in sample bias.
Conclusion:
The CHIP curriculum centers around incorporating a plant-based diet with proper patient education to prevent chronic diseases. Studies have shown that a plant-based diet reduces risk of atherosclerosis, coronary artery disease, and other cardio-metabolic diseases due to the absence or lowering intake of animal fat and carbohydrates.11,12 A plant-based diet alone cannot adequately change the behavior of patient;13 instead, what CHIP does well is the educational component that promotes nutrition that allows patients to understand the harms and benefits of their food choices in their health. Other components that could be adjusted at SLCH’s CHIP include: (1) incorporation of participants’ support system; (2) dietitian follow-ups with patients six months and a year after completion of the program; (3) use of exercise rooms at SLCH to incorporate exercise routine to the curriculum; (4) post-course surveys for participant feedback regarding the course.
The data from two years of CHIP at SLCH showed positive short-term effects of decreasing cholesterol, HDL, LDL, BP systolic, BP diastolic, weight, and fasting glucose. These results validate the already established findings of plant-based diet in the reduction of health risks. It also highlights the importance of patient education when implementing changes in patients’ lifestyle. The CHIP intervention, which revolves around a plant-based diet along with an emphasis and education on personal lifestyle choices to overall health, shows a positive short-term reduction in risk factors that contribute to chronic diseases within the Samaritan Health Services and the Linn County population.
Further research should explore the long-term effects of the CHIP in reducing health risks with suggestions laid out for the SLCH program.
Acknowledgments:
Thank you to the Samaritan Health Services staff members that conducted the CHIP, for their dedication in quality health care and to the statisticians at Samaritan Health Services, for their help in data analysis.
References:
- Anderson G. Chronic Care: Making the Case for Ongoing Care (pp. 1–44). Robert Wood Johnson Foundation website. https://www.rwjf.org/content/dam/farm/reports/reports/2010/rwjf54583. Published 2010.
- Cecchini M, Sassi F, Lauer JA, Lee YY, Guajardo-Barron V, Chisholm D. Tackling of unhealthy diets, physical inactivity, and obesity: Health effects and cost-effectiveness. The Lancet. 2010;376(9754):1775–1784. https://doi.org/10.1016/S0140-6736(10)61514-0.
- Drozek D, Diehl H, Nakazawa M, Kostohryz T, Morton D, Shubrook JH. Short-Term Effectiveness of a Lifestyle Intervention Program for Reducing Selected Chronic Disease Risk Factors in Individuals Living in Rural Appalachia: A Pilot Cohort Study. Advances in Preventive Medicine. 2014;798184. https://doi.org/10.1155/2014/798184.
- Kent L, Morton D, Hurlow T, Rankin P, Hanna A, Diehl H. Long-term effectiveness of the community-based Complete Health Improvement Program (CHIP) lifestyle intervention: A cohort study. BMJ Open. 2013;3(11):e003751. https://doi.org/10.1136/bmjopen-2013-003751.
- Leibold C, Shubrook JH, Nakazawa M, Drozek D. Effectiveness of the Complete Health Improvement Program in Reducing Risk Factors for Cardiovascular Disease in an Appalachian Population. The Journal of the American Osteopathic Association. 2016;116(2):84–91. https://doi.org/10.7556/jaoa.2016.020.
- Morton D, Rankin P, Kent L, Dysinger W. The Complete Health Improvement Program (CHIP): History, Evaluation, and Outcomes. American Journal of Lifestyle Medicine. 2014;10(1):64–73. https://doi.org/10.1177/1559827614531391.
- Acharjee S, Boden WE, Hartigan, PM, et al. Low levels of high-density lipoprotein cholesterol and increased risk of cardiovascular events in stable ischemic heart disease patients: A post-hoc analysis from the COURAGE Trial (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation). Journal of the American College of Cardiology. 2013;62(20):1826–1833. https://doi.org/10.1016/j.jacc.2013.07.051.
- Rosenson RS, Durrington P. HDL cholesterol: Clinical aspects of abnormal values [Medical education]. UpToDate website: https://www.uptodate.com/contents/hdl-cholesterol-clinical-aspects-of-abnormal-values. Published 2017. Accessed August 20, 2019.
- Ko DT, Alter DA, Guo H, et al. High-Density Lipoprotein Cholesterol and Cause-Specific Mortality in Individuals Without Previous Cardiovascular Conditions: The CANHEART Study. Journal of the American College of Cardiology. 2016;68(19):2073–2083. https://doi.org/10.1016/j.jacc.2016.08.038.
- Bartlett J, Predazzi IM, Williams SM, et al. Is Isolated Low High-Density Lipoprotein Cholesterol a Cardiovascular Disease Risk Factor? New Insights From the Framingham Offspring Study. Circulation. Cardiovascular Quality and Outcomes. 2016;9(3):206–212. https://doi.org/10.1161/CIRCOUTCOMES.115.002436.
- Kent L, Morton D, Rankin P, et al. The effect of a low-fat, plant-based lifestyle intervention (CHIP) on serum HDL levels and the implications for metabolic syndrome status – a cohort study. Nutrition & Metabolism. 2013;10;58–58. https://doi.org/10.1186/1743-7075-10-58.
- Tuso P, Stoll SR, Li WW. A plant-based diet, atherogenesis, and coronary artery disease prevention. The Permanente Journal. 2015;19(1):62–67. https://doi.org/10.7812/TPP/14-036.
- Null G, Pennesi L. Diet and lifestyle intervention on chronic moderate to severe depression and anxiety and other chronic conditions. Complementary Therapies in Clinical Practice. 2017;29:189–193. https://doi.org/10.1016/j.ctcp.2017.09.007.
Article information:
Published Online: Sept 6th, 2020.
IRB Approval: The methods used in this study were approved by the Western University of Health Sciences Institutional Review Board (Reference #18077)
Conflict of Interest Declaration: There are no conflicts of interest that the authors have to disclose.
Funding Source/Disclosure: No funding was allocated for this study.