Anita Rao1, Saumil Mehta2
PNWMSRJ. Published online Oct 15th, 2020.Abstract
A narrative literature review was conducted to ascertain the efficacy of manual manipulation for the treatment of plantar fasciitis (PF). PF is a common painful condition of the plantar foot. The current literature on the pathophysiology of PF is veering from inflammatory towards degenerative, making it an apt target for manual medicine. Osteopathic manipulative techniques (OMT) offer safe yet effective treatment methods to halt or delay the deformation to the plantar fascia thereby preventing its degradation. Our goals with this literature review are to provide a review of the existing Osteopathic manipulative techniques to treat Plantar Fasciitis and to encourage further data driven research for the use of OMT for Plantar Fasciitis.
Introduction
Plantar fasciitis (PF) is a prevalent condition treated among podiatrists, osteopathic and allopathic physicians, chiropractors, and physical therapists. It often presents as heel pain and 10 percent of individuals in the United States will experience PF at some point in their life.1 There are as many as 1 million cases diagnosed with plantar fasciitis yearly.2 The incidence rate of PF increases with an increase in age, the most common age to experience plantar fasciitis is when the individual is 40-60 years old.3 Despite this high incidence rate, treatment for PF varies among these providers considerably. This variation in treatment makes the diagnosis and management of PF challenging for the patients as well as providers. Symptoms usually diminish within one year, but if they persist and non-invasive methods such as splints, orthotics, rest, shock wave therapy, and injections are not effective surgery is generally considered. The use of manual medicine techniques independently or in conjunction with current techniques could help prolong non-invasive management of PF and yield better outcomes.
Manual manipulation is one of the oldest treatments and has been used globally within various professions including, osteopathic physicians, podiatrists, chiropractors, physical therapists, and massage therapists. Although there is a plethora of information and evidence around the effectiveness of manual manipulation each field has unique names for the same treatment. The use of several different names creates distinctions between each field scattering the studies conducted and thereby blocking off the interpretation of their results from other fields’ providers. We have compared the efficacy of manual treatments, such as counterstrain, myofascial release, and HVLA within the osteopathic, podiatric, chiropractic, and physical therapy fields. Compiling the results of studies and grouping them under shared terminology may aid in furthering the understanding of the procedures, efficacy, and best use of manual medicine. The potentially significant benefits of manual medicine are associated with minimal risks for the patient, and thus make it a logical solution to be incorporated into the care of physicians and therapists.
Methods
The main electronic databases used for this literature review was PubMed and Google Scholar. The keywords utilized for the search were: “OMM for plantar fasciitis”, “conservative treatments for plantar fasciitis”, “osteopathic treatment for plantar fasciitis”, “ counterstrain for plantar fasciitis”, “osteopathic approach to plantar fasciitis”, “myofascial release and plantar fasciitis”, “conservative treatment for plantar fasciitis”, “MFR for plantar fasciitis”, “HVLA for plantar fasciitis”, “Anterior talar dysfunction and plantar fasciitis”, “muscle energy for plantar fasciitis”, “electric shock wave therapy”, “strain-counterstrain for plantar fasciitis”, “plantar fascial stretching”, and “corticosteroid injection for plantar fasciitis”.
We screened the articles through the title, abstract, summary, and date published. We found several scientific studies which were designed as randomized clinical trials looking specifically at the effects of OMM on patient outcomes with plantar fasciitis. Other studies compared OMM to static stretching and conventional physical therapy exercise. We included articles discussing possible standard treatment protocols for treating plantar fasciitis. Certain articles we reviewed had animal studies included within it.
Counterstrain
Counterstrain is an osteopathic manipulative medicine technique in which the practitioner diagnoses the patient’s somatic dysfunction through identifying non-radiating tender points and passively positions the patient to decrease the tenderness of the point.4 By passively positioning the tissue to approximate the bony attachments of muscle the practitioner is taking advantage of natural neuromuscular reflex arcs to relax tissues.3 When the tissue is able to relax in the position of injury or strain the reflex arcs are attenuated and the pain signals from the region are reduced. Deformation to tissue may initiate an inflammatory cascade releasing substance P. Prostaglandins may heighten and prolong this inflammatory response which result in the promotion of nociceptive activity resulting in increased sensitivity to touch. The goal of counterstrain technique is to normalize neurophysiologic functioning and correct a somatic dysfunction.4 The specific counterstrain points for plantar fasciitis are at insertion of the plantar fascia—at the calcaneus, as well as in the belly of the quadratus plantae muscle.3
The Flexion Calcaneus (FCA), also referred to as the quadratus plantae, is a tender point located on the plantar surface of the foot at the anterior end of the calcaneus, near the origin of the plantar fascia. This point can become tender after the onset of dysfunction and can be treated by counterstrain. The FCA tender point is likely related to dysfunction of the quadratus plantae. Patients with this tender point often present with symptoms of plantar fasciitis or even plantar fasciitis itself .4
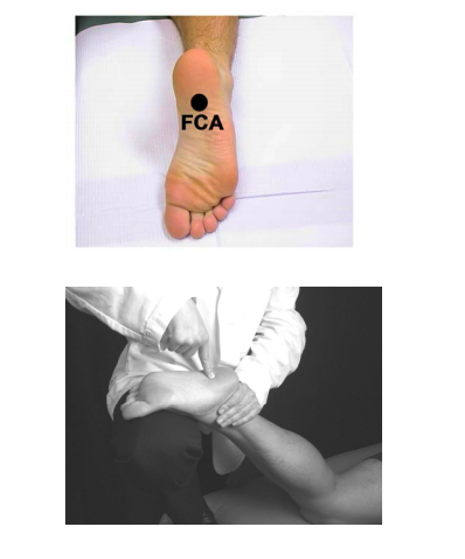
Figure 1. Tender point location (above) and treatment position (bottom)
Images reproduced with permission from WesternU OMM/NMM department
The efficacy of counterstrain specifically in relation to plantar fasciitis was tested in a randomized control trial by Wynee et. al. which concluded counterstrain OMM improves clinical outcomes for patients with plantar fasciitis compared to those who did not receive any OMM. The researchers found that the therapeutic effects came from mechanical improvements rather than electrical changes in reflex response of calf muscles. Additionally the researchers conducted a pretreatment and posttreatment symptom severity survey in which they found a significant relief in symptoms that was most pronounced immediately following treatment and lasted for 48 hours.5 Another study conducted by Pawar et al. determined that strain-counterstrain, synonymous to counterstrain, is effective in patients affected by plantar fasciitis and yielded improved ankle dorsiflexion range. In regards to pain the research subjects had a significant difference between pre and post intervention after 5 days of counterstrain therapy (p < 0.0001).6
MFR
Myofascial release (MFR) is an Osteopathic Manipulative treatment in which the physician identifies the spastic, resistant or tight myofascial tissue in an affected region of the body and precedes to engage that area by applying gentle sustained pressure. By doing so will allow the patient to restore motion.4 MFR can be done either directly or indirectly. Direct MFR involves directly engaging the restrictive myofascial barrier and applying constant force until there is a release of the tensed tissue. Indirect MFR involves moving the dysfunctional tissues in the direction of ease until increased movement is sensed.4
The efficacy of MFR in management of plantar fasciitis was examined in a randomized controlled trial. This study measured outcomes using the foot functional index. Sixty-six patients diagnosed with plantar fasciitis were randomized and put into the control group(sham ultrasound therapy) and experimental group(MFR). This study concluded that MFR was more effective than the sham ultrasound therapy for the treatment and management of plantar fasciitis.7 The study also broadly concluded that a large number of people can benefit from MFR that are suffering from plantar fasciitis.7 Another study set out to examine the differences within OMM techniques (MET vs MFR)and patient outcomes. The patient outcomes were measured using visual analog scale(VAS), foot and ankle ability measure(FAAM), and foot functional index(FFI). There were a total of 30 patients divided into two groups. One group received Muscle Energy Technique and the other group received MFR. They found no significant differences between the two groups and concluded that both MET and MFR were effective in reducing pain and improving lower limb function.8
HVLA
High Velocity Low Amplitude (HVLA) is an OMM technique in which the practitioner applies a direct rapid force over a short distance to joints which exhibit signs of a treatable somatic dysfunction. One of the oldest uses of manual medicine and the the most frequently used techniques amongst osteopathic physicians, chiropractors, and physiotherapists has been the manipulation of the spine, pelvis, and peripheral joints.4 In the lower extremities these methods can correct misalignment and malrotation of bones. Misalignment, especially in the foot, ankle, and leg can disrupt normal tensions in tendons and ligaments.3 Addressing any misalignment of bones may help decrease foot pain, as the bones of the foot represent key areas of focus in foot pain, in particular plantar fasciitis, because of their ligamentous and muscular attachments within the arches.3 Misalignments can occur at the talus bone, specifically if it is flexed in can cause restriction in dorsiflexion of the talus and this ankle as a whole.4 Another joint dysfunction of the ankle involves the tarsal bone. Displacement of the tarsal bone can cause eversion of navicular bone, inversion of cuboid bone, dorsal arching of cuneiform bones. These corresponding changes lead to the resistance of plantar arching which may be involved in the development of symptoms in plantar fasciitis. Talus and Talar HVLA are two HVLA techniques that can be used to address possible plantar fasciitis dysfunction.
In a study conducted by Dimou et al. chiropractic adjustments of foot and ankle subluxations with archwear compared to shock absorbing orthotics custom designed by a podiatrist. The chiropractic adjustments occurred twice weekly for four weeks and once at the one month follow-up. The custom orthotics included a range of subtalar, midtarsal and neutral casts and they were worn for eight weeks. On day 15 there was a significant difference in pain ratings between the interventions, favoring chiropractic adjustments with stretching over orthotics, however both groups saw significant improvements in pain rating, first step pain, heel pain during leisure, and algometer measurements. Furthermore, there were no adverse events reported in either group.9 The results from this study highlight the possibility that conducting manual manipulation of the joints affected independently or in conjunction with orthotic therapy may yield more long term and efficacious results than orthotic therapy alone. One such chiropractic treatment that can be used is the activator treatment on calcaneal subluxations which have proven to successfully manage symptoms in patients with plantar fasciitis and heel spurs.10 The activator treatment is in theory a high velocity low amplitude (HVLA) thrust delivered to a bone, but rather than the chiropractor using their hands the provider uses an instrument called the activator which delivers the thrust.
Moreover, HVLA may be useful in the event that a patient has new or recurring pain after surgery to relieve plantar fasciitis. A case report of fifteen patients found that patients who had unmanageable foot pain after plantar fascia release surgery, plantar fasciotomy, benefited from joint mobilization and manipulation. The study also concluded that joint mobilization and/or high velocity, low amplitude manipulation are safe conservation procedures to use in the treatment of patients with lateral column foot pain in status post fasciotomy.11
Conclusion
Our review of the current literature surrounding manual manipulation and the treatment of plantar fasciitis has highlighted the need for a broader understanding of the treatments used and the order in which they are employed. Osteopathic manipulative medicine has proven to be an effective conservative treatment. This review has compiled the various literature currently available on manual manipulation and its use in treating plantar fasciitis. The aim of this review is to provide a concise resource for providers to curate their own protocols from. A considerable amount of research has been done on the effectiveness of osteopathic and other manipulative medicine, which points to the potential vital role it may have in delaying or preventing the need for surgery in many patients, as well as, provide immediate relief of symptoms. This review highlights the need to develop a standard protocol to treat and manage plantar fasciitis, in which the naming of techniques manual manipulation should be standardized. Such standardization would allow data among osteopathic, chiropractic, podiatric, and therapists alike to be shared and interpreted with greater ease.
Future research should target the efficacy rates of the various manual medicine techniques in comparison to traditional methods employed today. Although this process may be cumbersome it is vital to understanding the specifics of how long and how frequently treatments must be performed to be effective long term. With a greater pool of data it will be easier to compare the long term effects of the various treatment methods employed to treat plantar fasciitis.
References
- Scher DL, Belmont PJ, Owens BD. The epidemiology of plantar fasciitis. Lower Extremity Review Magazine. https://lermagazine.com/article/the-epidemiology-of-plantar-fasciitis. Published April 2010. Accessed June 24, 2020.
- Petraglia F, Ramazzina I, Costantino C. Plantar fasciitis in athletes: diagnostic and treatment strategies. A systematic review. Muscles Ligaments Tendons J. 2017;7(1):107-118.
- Raghu Kanumalla MS, Keane JF, Matsushita S, Shoup D, Mauro AL, Goldstein L. Plantar Fasciitis: Diagnosis and Management. Practical Pain Management. https://www.practicalpainmanagement.com/treatments/manipulation/osteopathic/plantar-fasciitis-diagnosis-management. Published November 2018. Accessed June 18, 2020
- Osteopathic Principles and Practice: Osteopathic Manipulative Treatment. Pomona, CA. Department of Neuromusculoskeletal Medicine/Osteopathic Manipulative Medicine, Western University of Health Sciences,College of Osteopathic Medicine of the Pacific, 2019-2020.
- Wynne MM, Burns JM, Eland DC, Conatser RR, Howell JN. Effect of counterstrain on stretch reflexes, hoffmann reflexes, and clinical outcomes in subjects with plantar fasciitis [published correction appears in J Am Osteopath Assoc. 2006 Nov;106(11):636]. J Am Osteopath Assoc. 2006;106(9):547-556.
- Pawar PA, Tople RU, Yeole UL, Gharote GM, Panse RB, Kulkarni SA. A study on effect of strain-counterstrain in plantar fasciitis. Int J Adv Med. 2017;4(2):551-555.
- M S, Ajimsha & Binsu, Daniel & Chithra, S.. (2014). Effectiveness of Myofascial Release in the Management of Plantar Heel Pain: A Randomized Controlled Trial. The Foot. 24. 10.1016/j.foot.2014.03.005
- Chitara V, .International Journal of Science, Research (IJSR). To compare the effectiveness of muscle energy technique versus myofasial release in pain and lower limb functional activity in subjects having planter fasciitis – A randomized control trial. Ijsr.net. https://www.ijsr.net/get_abstract.php?paper_id=ART20172019. Accessed July 22, 2020
- Stuber K, Kristmanson K. Conservative therapy for plantar fasciitis: a narrative review of randomized controlled trials. J Can Chiropr Assoc. 2006;50(2):118-133
- Gleberzon BJ. Chiropractic “Name Techniques”: a review of the literature. The Journal of the Canadian Chiropractic Association. 2001;45(2):86
- Wyatt LH. Conservative chiropractic management of recalcitrant foot pain after fasciotomy: a retrospective case review. J Manipulative Physiol Ther. 2006;29(5):398-402. doi:10.1016/j.jmpt.2006.04.005
Article information:
Published Online: Oct 15th, 2020.
IRB Approval: IRB approval was not necessary for the composition of this article.
Conflict of Interest Declaration: The authors declare that there is no conflict of interests.
Funding Source/Disclosure: The Authors declare that no support was provided.