Caroline Baber 1, Mandilin Hudson, DO1
PNWMSRJ. Published online November 2nd, 2021.Abstract:
COVID-19 first was discovered in the United States in January 2020 and has since changed the way we live. From donning PPE to social distancing to virtual workplaces, we have all been affected by this pandemic. Those working on the front lines have been particularly impacted. The goal of this study is to assess the changes in mental health status among first responders as a result of COVID-19, thus allowing organizations to implement systemic changes as needed to help their employees.
Average anxiety levels increased significantly from 1.8 to 4.9 (p = 0.019) following the onset of the pandemic on February 28, 2020, correlating to a clinical anxiety level rise from mild to moderate. Depression levels increased significantly from 0 to 1.3 (p = 0.037), however this does not correlate to a clinically significant screening as depression scores remained in the no depression range. From this data, we can conclude that COVID-19 has negatively impacted the mental health of first responders within LFD – especially regarding anxiety levels. However, more data is recommended due to the small sample size. From this knowledge, first responders and their employers should implement changes to increase mental health care and wellness as mental health disorders can lead to lower life expectancies and poorer physical health outcomes.
Background:
Early research conducted on mental health within the scope of COVID-19 in China found that 54% of health care workers reported the psychological impacts of the pandemic to be moderate or severe with 29% reporting moderate to severe anxiety as a result2. This is significant because people with an established mental health disorder have lower life expectancies and poorer physical health outcomes when compared to the general public3.
First responders are faced with additional mental health challenges as the first people on scene. They see the full impacts of trauma before any medical care can be rendered and often are faced with severe triage situations, having to prioritize the lives of those that can be saved given their resources. This can further contribute to mental health disorders – something that was brought to light following the September 11, 2001 terrorist attacks in New York.
The goal of this study was to analyze the effects of COVID-19 on the mental health of firefighters and EMS workers within the Lebanon Fire Department – a rural fire and EMS service consisting of approximately 35 full time employees and 80 volunteers. Using questions from the General Anxiety Disorder 7 (GAD-7) questionnaire and Patient Health Questionnaire 2 (PHQ-2), first responders were asked to assess their mental health both before and after the COVID-19 outbreak in Oregon. This allowed us to quantify the changes in mental health status among first responders thus allowing organizations to implement systemic changes as needed to help their employees. We hypothesized that COVID-19 negatively impacted mental health among first responders correlating with increasing scored on the GAD-7 and PHQ-2 screening tools.
Materials and Methods:
An anonymous online survey was administered to first responders – defined as firefighters, EMTs, and paramedics – within the Lebanon Fire Department. Participants were asked to access their mental health using GAD7 and PHQ2 screening tools both pre- and post-the onset of COVID-19 in Oregon, defined as February 28th, 2020. Data was collected during November 2020 and used recall to access pre-pandemic scores. Previous mental health disorders and deliberate wellness activity participation – including counseling, support groups, exercise, etc. – were also investigated. Pre- and post-pandemic GAD7 and PHQ2 scores were analyzed using Wilcoxon rank sum tests for non-parametric data with a significance level of 0.05. All analysis was performed in R version 4.0.3.
Discussion:
Anxiety and depression have significant impacts on the overall health of those affected, correlating to lower life expectancies and poorer physical outcomes3. Therefore, it is important that we evaluate the impacts of mental health on those around us. It was found that first responders had increases in both anxiety and depression screening tools in response to the COVID-19 pandemic. From this information, we can conclude that COVID-19 has had a negative impact on the mental health of first responders.
Depression levels, while increased among first responders post-pandemic onset, did not show a clinically significant increase as levels remained at no depression. However, the sample size of this study was small (n=13) and repetition on a larger scale may show different results. This study has the potential for recall bias when assessing pre-pandemic anxiety and depression levels as participants were asked to access their pre-pandemic levels many months after the onset of COVID-19. Additionally, this study was conducted in the first few months following the onset on COVID-19 and results obtained now may show more significant impacts.
Table 1. Effects of participation in deliberate wellness activities– including counseling, support groups, exercise, etc. – on average GAD7 scores pre-pandemic, post-pandemic, and the change in these scores. Average change in GAD7 score p-value = 0.3367 (alpha = 0.05), n=13.
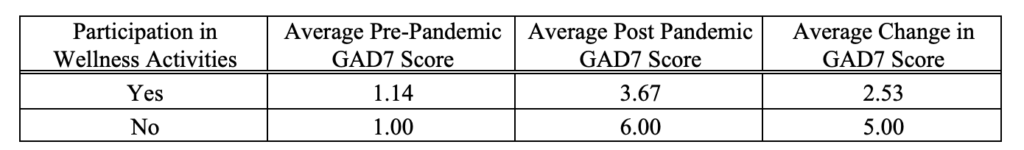

Figure 1. Changes in GAD7 scores pre- and post-pandemic onset.

Figure 2. Comparison of average GAD7 score for first responders within LFD pre- and post- pandemic. P value = 0.019 (alpha = 0.05), n=13.

Figure 3. Comparison of average PHQ2 score for first responders within LFD pre- and post- pandemic. P value = 0.037 (alpha = 0.05), n=13.
Results:
Average anxiety increased significantly from 1.8 to 4.9 (p value = 0.019) following the onset of the pandemic on February 28, 2020 (Fig. 2). This correlates to a clinical anxiety level rise from mild to moderate. For 11 of the 13 individuals assessed in this study, GAD7 scores increased with the most significant being a jump from a GAD7 score of 0, corresponding to no anxiety, to a GAD7 score of 15, corresponding to severe anxiety (Fig. 1).
Conclusion:
As many as 18% of adults in the United States demonstrate some form of anxiety or depression [1] – diseases which can be amplified by acute stressors such as COVID-19. For those working as first responders, it is important that we are not only aware of mental health disorders but help provide those affected with resources to lessen the burden. Though this study only assessed the Lebanon Fire Department, it is likely that other departments would yield similar results in response to anxiety and depression levels. From this knowledge, first responders and their employers should implement changes to increase mental health care and wellness during this particularly stressful time.
Acknowledgements:
Thank you to the Lebanon Fire Department for agreeing to participate this study as well as Johannie Spann for her help with data analysis.
References
- Carek, P. J, S. Laibstain, S. Carek. “Exercise for the treatment of depression and anxiety”. The International Journal of Psychiatry in Medicine. 2011;41(1):15-28.
- Cullen W., G. Gulati, B.D. Kelley. “Mental health in the Covid-19 pandemic”. Oxford University Press Public Health Emergency Collection. March 30, 2020.
- Rodgers, M., J. Dalton, M. Harden, A. Street, G. Parker, A. Eastwood. “Integrated care to
address the physical health needs of people with severe mental illness: a mapping review of the recent evidence on barriers, facilitators, and evaluations”. International Journal of Integrated Care. 2018. - Smith, Erin C., Lisa Holmes, Frederick M. Burkle Jr. “The physical and mental health challenges experienced by 9/11 first responders and recovery workers: a review of literature”. Prehospital Disaster Med. 2019;00(00):1-7.
Article information:
Published Online: November 2nd, 2021.
IRB Approval: The methods used in this study were approved by the Western University of Health Sciences Institutional Review Board (Reference # X20/IRB/068)
Conflict of Interest Declaration: There are no conflicts of interest to disclose.
Funding Source/Disclosure: No funding was allocated for this study.