Brandon Bealer1, Logan Leavitt1, Richard Bell1, Andrew Ambler DO
PNWMSRJ. Published online Oct 3rd, 2020.Abstract:
Background: Gout is a common arthritic joint disease that predominantly presents in the first metatarsophalangeal joint. It is caused by the deposition of monosodium urate crystals in the joint causing pain, inflammation, and swelling. The clinical manifestations of acute gout include severe joint pain, edema, and erythema. Case Presentation: A 68-year-old Caucasian female presented with lower back pain with associated myalgias, malaise, and intermittent dyspnea. On exam, she was febrile with decreased breath sounds and 1+ bilateral lower extremity edema. The patient was diagnosed with spinal gout and began prednisone therapy. Conclusion: The analysis of our case report suggests that physicians should consider the diagnosis of spinal gout in patients with nonspecific back pain and a history of chronic gout. Although it is rare for gout to disseminate into the spine, it is important to remember that gout is caused by an increased level of urate in the bloodstream and may deposit anywhere in the human body.
Introduction:
Gout is the most common type of inflammatory arthritis. The prevalence of gout in the United States among adults was recently found to be 3.9%.1 It is caused by the deposition of monosodium urate crystals in a joint causing pain, inflammation, and swelling. Gout is more common in males with a particular predominance in Caucasian males.1
The clinical manifestations of acute gout include severe joint pain, edema, and erythema. The onset of pain is generally within 24 hours and often resolves within 7-14 days.2 Chronic manifestations include nodules, prolonged inflammation, joint damage, and arthritis. Acute on chronic attacks are common, even in patients receiving gout prophylaxis.3
We present the case of a patient with a history of gout with severe back pain without any other joint pain. During the course of treatment, an acute gouty flare appeared. A course of colchicine and steroids resolved the acute gouty flare as well as the associated back pain. To the best of our knowledge, there are no other similar cases in the medical literature.
Case Presentation:
We present the case of a 68-year-old Caucasian female, with a past medical history of congestive heart failure, chronic kidney disease, and gout who presented with uncontrolled, acute on chronic back pain. The pain was described as spasm-like and rated as an 8 out of 10 in severity. Associated symptoms included one episode of urinary incontinence, feelings of malaise, myalgias, and intermittent dyspnea. The patient denied dysuria, hematuria, cough, and chest pain. The patient reported a history of back pain and a past medical history of sciatica.
Examination revealed an easily arousable, morbidly obese female. Vitals were a blood pressure of 103/55 mmHg, heart rate of 69 bpm, respiratory rate of 18, oxygen saturation of 97% on room air, and a temperature of 38.4 degrees Celsius. Auscultation of the heart revealed an irregularly irregular rhythm and a 3/6 systolic murmur. The pulmonary exam revealed un-labored breathing with diminished breath sounds in the lung bases bilaterally. Extremity examination revealed 1+ bilateral lower extremity edema. The rest of the examination was unremarkable.
Laboratory testing revealed a white cell count of 19.7 x 109 /l (4-11 x 109 /l). Serum sodium was 133 mEq/L (136-145 mEq/L), serum chloride 92 mEq/L (95-105 mEq/L), and serum bicarbonate 32 mEq/L (22-28 mEq/L). Serum urea nitrogen 72 mg/dL (7-18 mg/dL) and serum creatinine 1.53 mg/dL (0.6-1.2 mg/dL). Serum aspartate aminotransferase 46 U/L (8-40 U/L). Urinalysis revealed blood, leukocyte esterase, and 3+ monosodium urate. Procalcitonin was 1.5 ng/mL (0.10-0.49 ng/mL). Due to the elevated levels of procalcitonin, along with abnormal urine study, a concern of sepsis was considered, and infectious disease was consulted.
A computed tomography (CT) scan of the lumbar spine region was performed (fig 1). The scan showed enhancement in the L4-5 region related to inflammation but was non-specific. A magnetic resonance imaging (MRI) exam of the lumbar spine was performed as well (fig 2). Magnetic resonance imaging (MRI) of the lumbar spine revealed epidural enhancement with early phlegmon in the area of spinal segments L4-S1. There was a loss of disc height in the L2-L5 regions and mild disc bulging at the vertebral level of L2-S1 with spinal stenosis and possible L5 nerve root impingement. An L5 bone biopsy, with cartilaginous tissue, was subsequently performed which revealed nonspecific reactive changes without any signs of inflammation or crystal deposition. A working diagnosis of discitis or osteomyelitis with epidural abscess was considered and the patient was administered empiric intravenous antibiotics with coverage of suspected pathogens.
The following day, the patient reported new-onset left wrist pain. Physical examination revealed left wrist inflammation and dactylitis of the right index finger. Needle aspiration of the wrist was performed demonstrating 3+ monosodium urate crystals. The patient was started on colchicine and prednisone medication therapy to improve gout-related symptoms in fingers and wrists. The following week, the patient demonstrated significantly decreased inflammation in the wrists and fingers as well as overall decreased back pain. A plan was made to slowly taper the prednisone and then start allopurinol to prevent the recurrence of gout. At the time of hospital discharge, the patient reported no back pain and was comfortable returning to her place of residence.
Discussion:
The initial presentation of our patient was uncontrolled, chronic back pain, and fever with a recent urinary tract infection (UTI) which led to the primary suspicion of a back infection with a possible ascending and metastatic infection to the spine. With the concern of systemic inflammatory response syndrome (SIRS) due to non-specific symptoms with prior UTI, procalcitonin levels were checked. Procalcitonin was elevated to 1.5ng/ml and the complete blood count (CBC) showed leukocytosis. The patient’s urinalysis was positive for leukocyte esterase, blood, and 3+ monosodium urate. Due to the patient’s history of gout, but no current common joint symptoms and renal failure, the 3+ monosodium urate level on urinalysis was not considered a clinically significant finding at the time. The patient was treated with intravenous antibiotics due to suspected infection and oxycodone for pain control. Despite the administration of pain medication, the back pain remained uncontrolled.
The patient had an acute gout flare the following day in the wrist and finger and was treated for that flare-up. Treatment rapidly improved the wrist and finger pain, as well as dramatic and quick improvement of her back pain. Although there was no diagnostic study showing uric acid crystals in the spine, the bone biopsy with cartilaginous tissue has limited use when diagnosing crystal associated arthritis (CAA). Looking at 65 synovial tissue biopsies from 1988 to 2015 with clinical suspicion of CAA, only 20% of the biopsies proved a positive result.4 Due to the patient presentation, CT and MRI tests showing enhancements, no signs of septic cause, and improvement with gout treatment, a clinical diagnosis of acute gouty discitis was made.
Epidemiological studies have shown that the incidence of gout is rising in the United States. 5 As the more cases increase, it is essential for physicians to recognize the abnormal presentations of gout. In 2015, 131 cases of reported spinal gout were reviewed, with 75% of patients having a history of gout and 59% with a current gout tophus within another joint. Diagnosis of spinal gout occurred with 75 of the patients requiring surgery for diagnosis and another 32 with bone biopsy or needle aspiration.6 In a retrospective study involving five cases of spinal gout between 2014 and 2017, only one of the patients avoided surgery in favor of conservative management and bone biopsy. A history of gout as well as an elevated uric acid level were associated with spinal gout in 4 of 5 patients.7
The analysis of our case report suggests that physicians should consider the diagnosis of spinal gout in patients with non-specific back pain and a history of chronic gout. Although it is rare for gout to disseminate into the spine it is important to remember that gout is caused by an increased level of urate in the bloodstream. Due to this fact, uric acid crystals can collect in virtually any part of the human body requiring blood supply. We also suggest that treatment with medications may be possible before surgery to decrease morbidities among patients. Further research should be completed in this area to provide improved diagnosis and treatment methods of spinal gout.
Learning Points:
- Spinal gout should be considered as a differential diagnosis in the workup of back pain in patients with a history of gout.
- Although gout classically presents in peripheral joints in the fingers and toes, remember that gout may disseminate and collect in various locations in the human body.

Figure 1. CT of the lumbar spine with enhancement of the L5-S1 disc space showing inflammation in the area
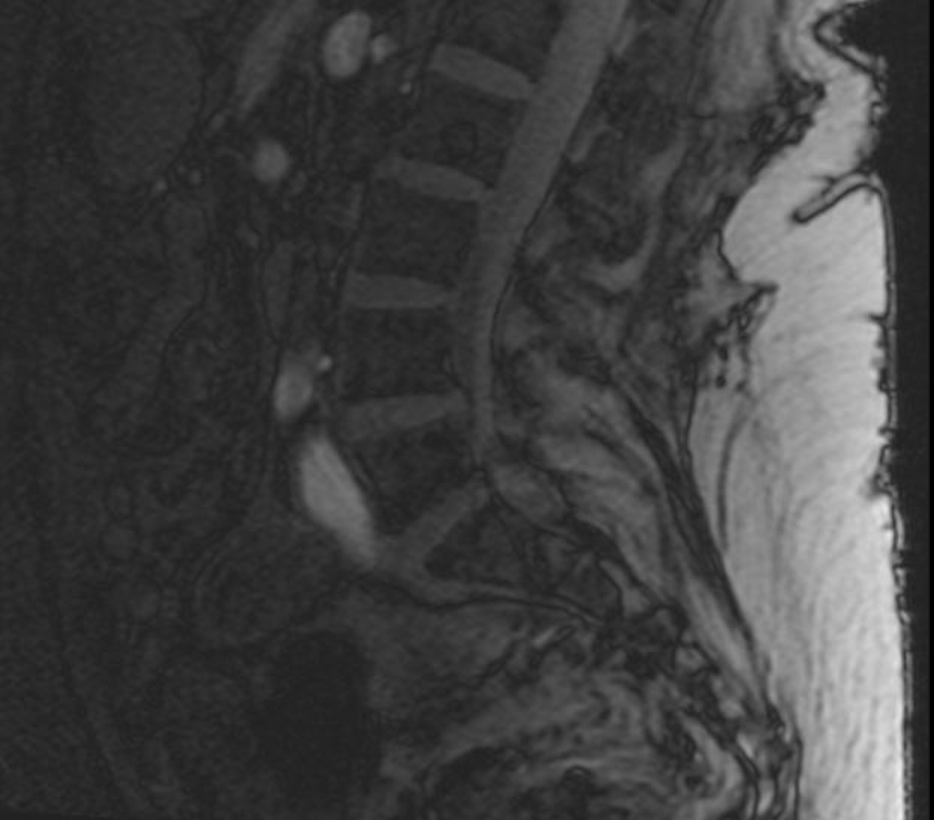
Figure 2. T-2 weighted MRI of the lumbar spine with enhancement in the L4-S1 region indicating early phlegmon.
References:
- Chen-Xu M, Yokose C, Rai SK, Pillinger MH, Choi HK. Contemporary Prevalence of Gout and Hyperuricemia in the United States and Decadal Trends: The National Health and Nutrition Examination Survey, 2007-2016. Arthritis Rheumatol. 2019;71(6):991-999.
- Hench PS. Diagnosis And Treatment Of Gout And Gouty Arthritis. JAMA: The Journal of the American Medical Association. 1941;116(6):453.
- Shiozawa A, Szabo SM, Bolzani A, Cheung A, Choi HK. Serum Uric Acid and the Risk of Incident and Recurrent Gout: A Systematic Review. J Rheumatol. 2017;44(3):388-396.
- Moses V, Asirvatham JR, Mchugh J, Ike R. Synovial Biopsy in the Diagnosis of Crystal-Associated Arthropathies. JCR: Journal of Clinical Rheumatology. 2020;26(4):142-146.
- Roddy E, Choi HK. Epidemiology of gout. Rheum Dis Clin North Am.2014;40(2):155-175.
- Toprover M, Krasnokutsky S, Pillinger MH. Gout in the Spine: Imaging, Diagnosis, and Outcomes. Current Rheumatology Reports. 2015;17(12).
- Ma S, Zhao J, Jiang R, An Q, Gu R. Diagnostic challenges of spinal gout. Medicine. 2019;98(16).
Article information:
Published Online: Oct 3rd, 2020.
IRB Approval: IRB approval was not necessary for this case report.
Conflict of Interest Declaration: The authors report no conflicts of interest.
Funding Source/Disclosure: No support or any source of funding was provided for this case report.